If you have breast pain, see your doctor to find out why you have pain and learn ways to manage it.
It is important to know that breast pain is
not a common symptom of breast cancer.
Assessing breast pain
To assess your breast pain, your healthcare provider will ask you about your breast health and family history, and then examine your breasts.
You may have a
mammogram,
ultrasound, or both tests to look for a possible cause for your pain.
Tell your healthcare provider:
- how long you have had the pain
- where the pain is
- what the pain feels like
- what brings on the pain
It's also helpful to tell your healthcare provider what you have tried to relieve the pain and what's worked or hasn't worked.
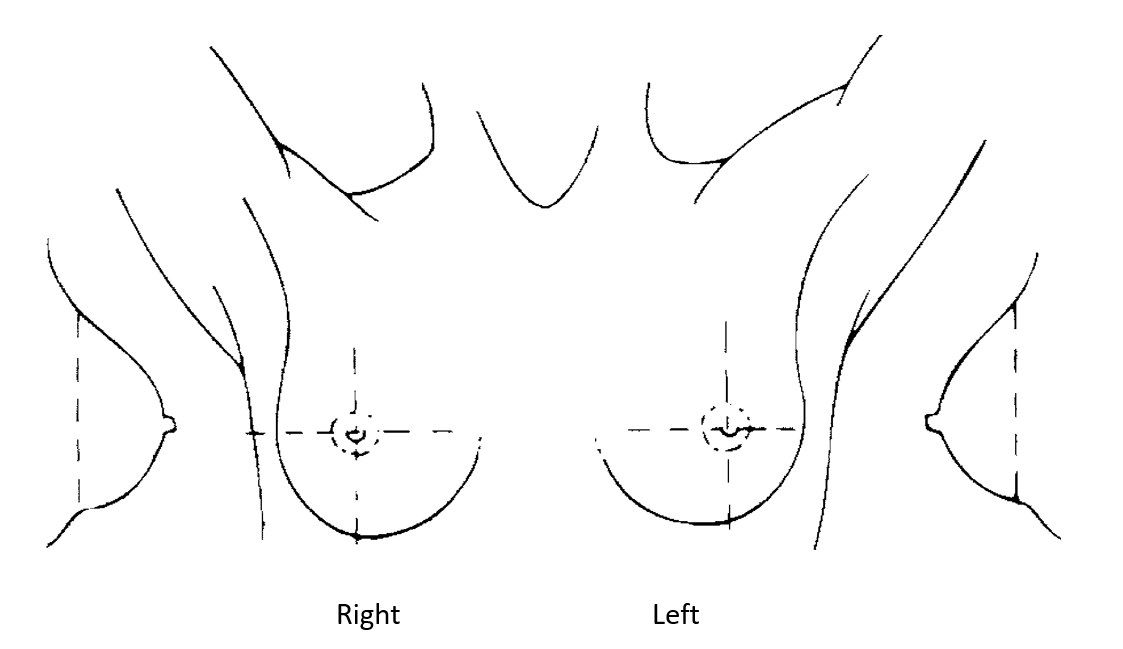
Breast map
Download and print the breast map below to help your healthcare provider assess your breast pain. Mark where you have pain in your breast or breasts. Mark if it is only on 1 side, on both sides, or in the armpit. Mark if the pain moves from 1 spot to another.
 Breast pain calendar
Breast pain calendar
It may help your healthcare provider find what's causing your pain if you keep a record for 3 to 4 months. Use this breast pain calendar to track your breast pain. When you use a scale of 0 to 10 (with 0 being no pain and 10 being the worst pain you can imagine), you or your healthcare provider may notice a pattern or link to your lifestyle or menstrual periods.
Types of breast pain
There are different types of breast pain. Your healthcare provider's assessment will tell you what type of pain you have.
Cyclical breast pain
Cyclical breast pain is related to your menstrual cycle. It is the most common type of breast pain. It is usually caused by regular hormone changes and happens in both breasts. It is generally described as feeling heavy or sore. The pain gets worse 1 to 2 weeks before your period and goes away when your period starts or soon after.
Cyclical breast pain happens more often in younger women and usually goes away at menopause.
Non-cyclical breast pain
Non-cyclical breast pain isn't related to your menstrual cycle. It may happen in 1 or both breasts. The pain may be sharp, burning, dull, achy, or throbbing.
Non-cyclical breast pain can have many causes, such as trauma, cysts, inflammation, infection,
fibroadenomas, medicines, heavy breasts, or clogged milk ducts. Treatment depends on the cause of the pain.
Chest wall pain
Chest wall pain (also called musculoskeletal pain) can often be mistaken for breast pain. Chest wall pain affects the muscles and soft tissues of the chest after a lot of exercise, an injury, or if the area between the ribs and breastbone gets inflamed.
Chest wall pain usually has no pattern. Physical activity can make the pain worse.
This pain often goes away in time. It is still important to see your healthcare provider to check the pain, especially if you have a heart condition or have had surgery or an injury in that area.
Managing breast pain
The following tips can help manage breast pain.
Wear a bra that fits
One of the most common causes of breast pain is wearing a bra that doesn't fit well. A bra that fits and has good support can help with breast pain. Get tips for fitting your bra. Some specialty bra stores that can help you find a bra that fits you best.
If you have breast pain, it's a good idea to wear a bra without underwire because the firm wire can make your pain worse.
If breast pain wakes you at night, try wearing a sports bra to bed.
Eat flaxseed
Some research shows that eating 2 tablespoons of ground flaxseed (not flaxseed oil) each day for 3 months helps lessen cyclical breast pain.
Use a topical anti-inflammatory medicine
If breast pain is in a specific area or is chest wall pain, putting an anti-inflammatory gel (for example, Voltaren Emugel) on your skin can help.
Ask your pharmacist about a non-prescription option. You can get a prescription for a stronger gel if you need it.
Have less caffeine and get regular exercise
Even though studies haven't proven that caffeine causes breast pain, you may find having less caffeine helps.
Regular exercise and activities that lower stress may help lessen breast pain.
Talk to your healthcare provider about the medicines you take
The birth control pill, hormonal intrauterine device (IUD), or hormone therapy can cause breast pain. Sometimes the pain goes away on its own after your body adjusts to the medicine.
If you think your pain is from the birth control pill or hormone therapy, talk to your healthcare provider. They may be able to switch you to a lower dose or to a different brand.
Other treatments
Your healthcare provider may recommend other treatments or medicines for your breast pain depending on the cause. Examples include:
- removing fluid from a cyst in the breast
- taking antibiotics if you have a breast infection
- changing the dose of your birth control pill or hormone therapy
- changing or stopping a medicine that could be making the pain worse
- prescribing medicines to help balance your hormones
- physiotherapy for chest wall pain
Herbal supplements and vitamins
There isn't enough evidence to recommend herbal supplements to treat breast pain.
Some supplements such as ginseng may cause breast pain. Research shows that vitamins A, E, and B6 don't help breast pain. Some vitamins such as vitamin A can even be toxic in large doses.
When to see your healthcare provider
See your healthcare provider if your breast pain:
- lasts longer than a few weeks
- is in 1 area of the breast
- is getting worse
- is spreading or changing
- is affecting your everyday activities
- is waking you up at night
- also comes with redness, a rash, or swelling
