Managing Your Pain After Surgery
Pain after surgery
Pain is part of the normal healing process after surgery. The first few days are usually the worst. Your pain should improve a little each day.
Managing your pain
When your pain is managed well, getting back to your usual activities after surgery will be easier. Pain control helps you take deep breaths and move around more. This helps you to heal faster and avoid some problems that can happen after surgery, like lung infection (pneumonia). It's normal to have some pain after surgery, even with pain medication. Pain medication may help you function better and cope with the amount of pain you have but often will not get rid of it entirely.
Your pain should be at a level that allows you to:
- be up and move around
- fall asleep
- do some of your normal activities
How do I know what to do to feel better?
There are many ways to treat pain including some that don't involve taking medications. You may go home with a prescription for pain medication. Some may contain opioids (narcotics), but others may not. You'll often be able to manage your pain with a combination of non-medication therapies and medications that don't contain opioids.
Some people have very little to no pain after surgery. If your pain gets better quickly use the suggestions for mild pain treatment. You may feel different levels of pain during the day. For example, your pain may be worse in the evening and less early in the day. Your pain should be getting better day by day, so you'll need less and less medication. If your pain doesn't get better or continues longer than expected, call your surgeon.
| How intense is my pain? | What can I do to feel better? |
|---|
Mild to moderate pain | I hardly notice my pain, and it doesn't interfere with my activities. | Non-medication therapy and Medications that don't have opioids You may take these to control mild to moderate pain as needed. Follow the dose instructions on the package. |
| I notice my pain and it distracts me, but I can still sit up, walk, and stand. |
Moderate pain | My pain is hard to ignore, and I notice it even when I rest. | Non-medication therapy and Medications that don't have opioids You may take these to control mild to moderate pain as needed. Follow the dose instructions on the package. |
| My pain interferes with my usual activities. |
Moderate to severe pain | I'm focused on my pain, and I can't do my daily activities. | Non-medication therapy and Medications that don't have opioids You may take these to control mild to moderate pain as needed. Follow the dose instructions on the package. and Short-acting opioids You should only need to take these for a few days. Call your surgeon if your pain is not getting less. |
| I'm groaning in pain, and I can't sleep. I'm unable to do anything. |
| My pain is as bad as it could be, and nothing else matters. |
Mild to moderate pain
Most people have good pain control with a non-steroidal anti-inflammatory drug (NSAID) and acetaminophen (Tylenol). You may not need anything stronger to manage your pain.
For the first 2 to 5 days take these pain medications whether you are hurting or not. Taking these medications regularly keeps a steady level of pain medication in your blood. This helps to keep your pain lower for longer. Use pain medication for up to 5 days based on how comfortable you feel and your ability to sleep and take care of yourself.
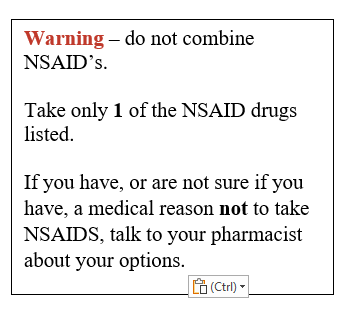
If you don't have allergies or other medical conditions that prevent you from taking these, you may take acetaminophen (Tylenol) and 1 of the options of NSAIDs. Ibuprofen (Advil, Mortin), ketorolac (Toradol) or naproxen (Aleve), and acetaminophen (Tylenol) can be safely taken together.
Non-medication therapy
There are 3 key things you can do to help with your pain. They include:
- self-care - involves getting rest, using an ice pack, and generally looking after yourself
- complementary therapy - can include guided imagery, meditation, and music
- movement - gentle exercise (moving), standing, and walking, first around your house and then outside as you're able
Non-opioid pain medication
Acetaminophen (Tylenol) - pain reliever, lowers pain and fever and is not habit-forming.
Do not use if you are allergic or have a sensitivity to this medication.
How much and how often?
You can take 650 to 1000 mg 4 times a day (24 hours) for at least 2 days but for no more than 7 days as needed. Take the lower dose (650 mg) if you are 65 years or older.
For regular strength take no more than 12 pills per day. For extra strength take no more than 8 pills per day (24 hours).
Common side effects:
- Nausea, vomiting, headache, and insomnia (can't sleep).
- Liver damage may occur at high doses (4000 mg in 24 hours). Don't take more than 4000 mg in 24 hours.
Non-steroidal anti-inflammatory drugs (NSAIDS)
Ibuprofen (Advil, Motrin), naproxen (Aleve), or ketorolac (Toradol) - These medications aren't habit forming, don't contain steroids, and lower swelling, inflammation, and pain. Taking this medication can help decrease the need for opioid pain medicine which can be habit-forming.
Do not use these if you are allergic or have a sensitivity to this medication.
How much and how often?
Ibuprofen (Advil or Motrin) - 400 to 800 mg 3 times a day (every 8 hours) for at least 2 days. Do not take more than 1200 mg in 24 hours.
Naproxen (Aleve) - 220 mg 2 times a day. Do not take more than 440 mg in 12 hours or 660 mg in 24 hours.
Ketorolac (Toradol) - 10 mg every 4 to 6 hours. Don't take more than 40 mg in 24 hours.
Common side effect:
Opioid medications
If you've had a more complex procedure or surgery, you may need to start on a combination of medications that includes opioids. Usually, prescribed opioid medication is only needed for up to 5 days. Take this medication as directed by your healthcare provider for your current surgery or procedure. Only use your opioid for acute after surgery pain.
For moderate to severe pain continue with non-medication therapy and non-opioid medications as needed.
If you have moderate to severe pain even with taking scheduled acetaminophen and 1 NSAID, you can take 1 of the following opioid medications:
- Hydromorphone 0.5 to 1 mg every 4 hours as needed
- Morphine 5 to 10 mg every 4 hours as needed
- Other: ____________________________
Other prescription medications that have opioids in them include:
- tramadol
- tramadol with acetaminophen (Tramacet)
- codeine with acetaminophen (Tylenol #3 or #4)
- morphine
- hydromorphone (Dilaudid)
- oxycodone
- oxycodone with acetaminophen (Percocet)
Only use the opioid medication for pain that is not managed with acetaminophen and 1 NSAID. Start to lower how much of the opioid you take as soon as your pain level becomes less.
If the opioid medication already contains acetaminophen (combination medication), don't take another dose of acetaminophen. Use the NSAID with the combination opioid medication.
Common side effects: nausea, dizziness, headache, drowsiness, slower rate of breathing, vomiting, dry mouth, itching, and constipation.
Serious side effects: very slow breathing (respiratory depression), overdose (taking too much of the medication), and death if your breathing is too slow or stops. Your risk of opioid abuse increases the longer you take the medication.
Tips for taking opioids safely:
- Lower your risk of creating a habit (addiction) by taking as little opioid pain medication as possible.
- Take opioids for the shortest amount of time. Using opioids beyond the suggested time can lead to it becoming a harmful habit. This can lead to other problems and may be fatal.
- Never take more medication than is prescribed.
- Do not drink alcohol while you’re taking NSAIDs or opioids.
- Take a stool softener to help prevent getting constipated. Talk to your pharmacist about over-the-counter stool softener options.
- Opioids can affect your ability to focus on your job. Talk to your surgeon or family doctor about when you can return to work.
- Driving - Do not drive for 24 hours after your surgery. Your surgeon will tell you if you need to stop driving for longer than 24 hours.
- Do not drive while taking your prescription pain medicine.
- Do not drive until you are able to move your arms normally and safely do a shoulder check.
Should I worry about becoming addicted to opioids?
There is always a risk with prescription opioids to become addicted. The risk for this is higher if you use opioids for something other than pain, for example, anxiety, sleep, fear of pain, or to feel good. Using more opioids than you need, longer than you need, or for reasons other than pain can create harmful habits or substance use problems.
Learn more about managing pain
- For up-to-date information about managing pain, pain medication, and treating your pain, go to MyHealth.Alberta.ca.
- For nurse advice and general health information anytime day or night, call Health Link at 811.
Safe use, storage, and disposal of prescription opioid medications
Opioids are high risk medications and may be fatal if not taken as prescribed. Improper use of opioid pain medication is a leading cause of accidental death.
Safe use
- Never take someone else’s opioid medications.
- Never give or sell your medication to someone else.
- Combining opioids with alcohol or other drugs increases the risk of death.
- Combining opioids with medication used to reduce anxiety can result in overdose.
Call your surgeon’s office during regular office hours if you have any questions about your pain medication.
Safe storage
Unused medications in your home are a risk for inappropriate drug use.
- Don’t keep leftover, unused, or expired opioid medication for use in the future.
- Keep opioids out of reach of children and pets. Also take steps to not make them available to teens and young adults. Wrongful or accidental ingestion can cause serious problems like harmful habits, addiction, overdose, and death.
- Hide or lock up opioid medications to avoid access by family, friends, or houseguests.
Safe disposal
When possible, return your leftover, unused, or expired medications to a pharmacy for proper and safe disposal. In Canada, you can return your unused and expired medication to any pharmacy any day of the year.
If no medication take-back program is available in your area, follow these simple steps to dispose of most medication in the garbage:
- Don't flush them down the toilet or sink.
- Take the medication out of their original containers. Scratch out all identifying information on the prescription label. This helps protect your identity and the privacy of your personal health information.
- Do not crush tablets or capsules.
- Mix medication with something unappealing, such as kitty litter or used coffee grounds. This makes the drug less attractive to children and pets, and unrecognizable to people who go through the trash looking for drugs.
- Place this mixture in a closed bag, empty can, or other sealed container to prevent the drug from leaking or breaking out of a garbage bag.
To see this information online and learn more, visit MyHealth.Alberta.ca/health/aftercareinformation/pages/conditions.aspx?hwid=custom.ab_managing_pain_after_surgery_adult_ac.
For 24/7 nurse advice and general health information call Health Link at 811.
Current as of: August 01, 2024
Author: Surgery Strategic Clinical Network, Alberta Health Services
This material is not a substitute for the advice of a qualified health professional. This material is intended for general information only and is provided on an "as is", "where is" basis. Although reasonable efforts were made to confirm the accuracy of the information, Alberta Health Services does not make any representation or warranty, express, implied or statutory, as to the accuracy, reliability, completeness, applicability or fitness for a particular purpose of such information.
