Condition Basics
What is thrush?
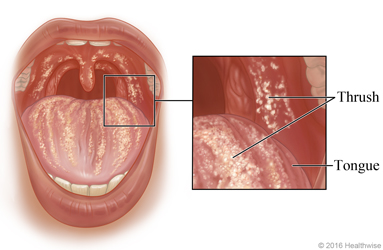
Thrush is a common infection of the mouth and tongue caused by the yeast Candida albicans. Thrush appears as white patches that look like cottage cheese or milk curds. When the patches are wiped away, the surface looks red and raw and may bleed.
What causes it?
Thrush occurs when a yeast grows out of control. Babies get thrush because their immune systems aren't strong enough to control the yeast's growth. Older people get thrush because their immune systems weaken with age. People who take certain medicines or have certain health problems are more likely to get thrush.
What are the symptoms?
The most common symptoms of thrush are white patches on the inside of the mouth and tongue. They look like cottage cheese or milk curds. Some babies may be cranky and may not want to eat. Adults may have a burning feeling in the mouth and throat or a bad taste in their mouth.
How is it diagnosed?
In most cases, doctors can diagnose thrush just by looking at the white patches. The doctor will also ask you questions about your or your child's health. If your doctor thinks that another health problem, such as diabetes, may be related to thrush, you may also be tested for that condition.
How is thrush treated?
In babies, thrush is usually treated with prescribed antifungal medicine such as nystatin liquid. In most cases, you will put the medicine directly on the white patches. The yeast can cause a diaper rash at the same time as thrush. Your doctor may prescribe nystatin cream or ointment for your baby's diaper area.
In adults, antifungal medicine that goes directly on the white patches, such as a liquid or lozenge, is usually tried first. If these medicines don't work, your doctor may prescribe an antifungal pill. People with weakened immune systems may need to keep taking antifungal medicine to prevent thrush.
Cause
You get thrush when a yeast called Candida grows out of control. Candida is normally found in small amounts in the mouth and other mucous membranes. It usually causes no harm. But when the yeast is able to grow uncontrolled, it invades surrounding tissues and becomes an infection.
- Babies get thrush because their immune systems aren't yet strong enough to control the growth of the yeast.
- Older people get thrush because their immune systems can weaken with age.
- Some people get thrush when they take certain medicines, such as antibiotics or inhaled corticosteroids.
- People who have certain health problems, such as diabetes or HIV, are also more likely to get thrush.
Prevention
In babies
Here are some tips for how to help prevent thrush in infants.
- Treat vaginal yeast infections, especially during the last 3 months of pregnancy.
This will decrease your baby's risk of getting thrush during delivery.
- Wash bottle nipples and pacifiers daily.
And keep all prepared bottles and nipples in the refrigerator to decrease the likelihood of yeast growth.
- Do not reuse a bottle more than an hour after the baby has drunk from it.
Yeast may have had time to grow on the nipple.
- Wash or boil all objects that the baby puts in their mouth.
Or run them through the dishwasher.
- Change your baby's diaper soon after it is wet.
A wet diaper area provides a good environment for the yeast that causes thrush to grow.
- Breastfeed your baby if possible.
Breast milk contains antibodies that will help build your baby's natural defence system (immune system) so your baby can resist infection.
- Contact your doctor with concerns about breastfeeding.
If your nipples become red and sore, or you have breast pain during or after nursing, it may be a sign that a thrush infection in your baby has spread to your nipples.
If your baby needs medicine to treat thrush, don't put the medicine dropper in the baby's mouth. Drop the medicine on a cotton swab and swab it on the affected area. Throw away the swab, and don't put anything back into the medicine bottle that could be contaminated with the yeast.
In adults
Here are some tips for preventing thrush.
- Practice good oral hygiene.
This includes brushing your teeth twice a day and flossing once a day.
- If you have had a previous thrush infection, replace your toothbrush to help prevent another infection.
- Take care of your dentures if you wear them.
Soak them each night in a chlorhexidine solution. You can get it from your pharmacist. You can also use a denture cleaner that is sold in most drug or grocery stores. Scrub your dentures with water both before and after soaking them. If you used chlorhexidine to soak your dentures, don't use fluoride toothpaste for at least 30 minutes after you put your dentures back in your mouth. (Fluoride can weaken the effect of chlorhexidine.)
- Practice good handwashing.
- Rinse your mouth with water soon after you take a liquid antibiotic.
Antibiotics can throw off the balance of bacteria in the mouth and can allow the growth of the yeast that causes thrush.
- Get treatment for conditions that increase your risk for thrush.
These include diabetes, human immunodeficiency virus (HIV), or cancer.
- Use a spacer when taking inhaled corticosteroids.
Rinse your mouth after you inhale the dose.
Learn more
Symptoms
In babies
Thrush can be a mild infection that causes no symptoms. If a baby has symptoms, they may include:
- White patches inside the mouth and on the tongue.
The white patches look like cottage cheese or milk curds. Thrush is often mistaken for milk or formula. The patches stick to the mouth and tongue and can't be easily wiped away. When rubbed, the patches may bleed.
- A sore mouth and tongue and trouble swallowing.
If the infant can't eat because of a sore mouth or throat, he or she may act fussy.
- Poor appetite.
The infant may refuse to eat, which can be mistaken for lack of hunger or poor milk supply.
- Diaper rash.
This may occur because the yeast that causes thrush also will be in the baby's stool.
In adults
Thrush can be a mild infection that causes no symptoms. If an adult has symptoms, they may include:
- A burning feeling in the mouth and throat.
This occurs at the start of a thrush infection.
- White patches that stick to the mouth and tongue.
The patches look like cottage cheese or milk curds. The tissue around the patches may be red, raw, and painful. If rubbed (during tooth brushing, for example), the patches and the tissue of the mouth may bleed easily.
- A bad taste in the mouth or trouble tasting foods.
Some adults say they feel like they have cotton in their mouth.
If you breastfeed, you may get a yeast infection of your nipples if your baby has thrush. This can cause sore, red nipples. You may also have a severe burning pain in your nipples during and after breastfeeding.
When to Call a Doctor
Call your doctor today if you or your child has been diagnosed with thrush and:
- You have symptoms that show the infection may be spreading, such as white patches on the skin outside of the mouth.
- Your symptoms are getting worse or have not improved within 7 days of starting treatment.
- Your symptoms come back often.
- You have HIV infection, cancer, or another condition that weakens your immune system.
Thrush in an infant's mouth can spread to the breast of the nursing mother. This can cause nipple redness and pain. Contact your doctor if you have redness and pain in the nipples in spite of home treatment or if you have burning pain in the nipple area when you nurse. Your doctor will likely examine your baby's mouth to find out if thrush is causing your symptoms.
Watchful waiting
If you have been diagnosed with thrush before and you believe you may have it again, home treatment may help. Very mild cases of thrush may clear up without medical treatment.
Check your symptoms
Treatment Overview
In babies
In healthy infants, thrush usually isn't a serious problem and is easily treated and cured. Except for the mildest cases, you should treat thrush to keep the infection from spreading.
Thrush is usually treated with prescribed antifungal medicine such as nystatin liquid. In most cases, you will put the medicine right on the white patches.
The yeast can cause a diaper rash at the same time as thrush. Your doctor may prescribe nystatin cream or ointment for your baby's diaper area.
Mild thrush is usually treated until at least 48 hours after the symptoms have gone away. For some severe infections, a longer treatment period may be needed.
In adults
Thrush is usually treated with antifungal medicines. These are either applied directly to the affected area (topical) or swallowed (oral).
Mild thrush
You will probably use antifungal medicine that goes directly on the white patches, such as a mouth rinse or a lozenge. Treatment usually lasts about 14 days.
Moderate to severe thrush
Thrush that spreads to the esophagus can cause a more severe infection. This is treated with antifungal pills. A topical antifungal medicine may also be used.
For some severe infections, treatment may last longer than 14 days.
Persistent or recurrent thrush
Persistent or recurrent cases of thrush may:
- Need to be treated twice as long as the symptoms last.
- Require treatment with both oral and topical medicines.
People with weakened immune systems may need to keep taking antifungal medicine to prevent thrush.
Self-Care
Caring for your child
- Clean bottle nipples and pacifiers regularly in boiling water.
- If you are breastfeeding, use an antifungal medicine, such as nystatin (Nyaderm), on your nipples. Dry your nipples after breastfeeding.
- If your child is eating solid foods, you can massage plain, unflavoured yogurt around the inside of your child's mouth. Check the label to make sure that the yogurt contains live cultures. Yogurt may help healthy bacteria grow in the mouth. These bacteria can stop yeast growth.
- Be safe with medicines. Have your child take medicines exactly as prescribed. Call your doctor or nurse advice line if you think your child is having a problem with any medicines.
- It's important to get rid of any sources of infection, or thrush will come back. Items your child may put in their mouth should be boiled or washed in warm, soapy water.
Caring for yourself
Here are some tips for managing thrush at home.
- Drink cold liquids.
Examples include water or iced tea. You can also eat flavoured ice treats or frozen juices.
- Eat foods that are easy to swallow.
Examples include gelatin, ice cream, or custard.
- If the thrush patches are painful, try drinking from a straw.
- Rinse your mouth several times a day with a warm saltwater rinse.
You can make the saltwater mixture with 1 tsp (5mL) salt in 1 cup (250mL) of warm water.
Learn more
Credits
Current as of: April 30, 2024
