Condition Basics
What is an ectopic pregnancy?
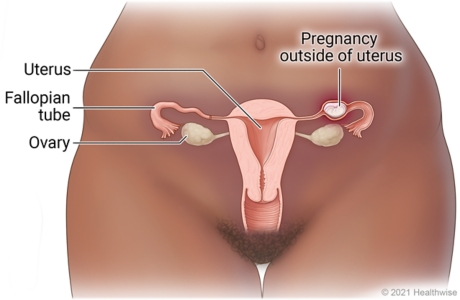
In a small number of pregnancies, the fertilized egg attaches to an area outside of the uterus, rather than in the uterus. This is called an ectopic pregnancy or extrauterine pregnancy.
Nearly all ectopic pregnancies develop in a fallopian tube. These are often called tubal pregnancies. If left untreated, a tubal ectopic pregnancy can cause fallopian tube damage and cause heavy bleeding that could be deadly. So unless the pregnancy is miscarrying on its own, medicine or surgery is used to treat the ectopic pregnancy.
Ectopic pregnancy can also occur in an ovary, the cervix, or the abdomen. This is rare.
What causes it?
An ectopic pregnancy is often caused by damaged fallopian tubes. A fertilized egg may have trouble passing through a damaged tube, causing the egg to implant and grow in the tube. Fallopian tube damage may be caused by things like pelvic inflammatory disease or smoking. Some ectopic pregnancies occur without any known cause.
What are the symptoms?
In the first few weeks, an ectopic pregnancy may cause the same symptoms as a normal pregnancy, such as a missed menstrual period, fatigue, nausea, and sore breasts.
The key signs of an ectopic pregnancy are:
- Belly, pelvic, or shoulder pain. It most often starts 6 to 8 weeks after a missed period. The belly pain may be sharp on one side at first and then may spread.
- Vaginal bleeding. It may be light.
How is it diagnosed?
A urine test can show if you are pregnant. If you have symptoms of a possible ectopic pregnancy, your doctor will likely do a pelvic exam, a blood test, and an ultrasound.
How is an ectopic pregnancy treated?
In most cases, an ectopic pregnancy is treated right away to avoid rupture and severe blood loss. Treatment may be medicine or surgery. Rarely, the doctor may recommend what's called expectant management. The decision about which treatment to use depends on how early the pregnancy is found and your overall condition.
What can help you cope after an ectopic pregnancy?
You may have many different emotions after an ectopic pregnancy. If you need help coping with any feelings, consider meeting with a support group. You also may want to read about others' experiences or talk with a friend, family member, or counsellor. If you're sad and it's not getting any easier, tell your doctor.
Cause
Fallopian tube damage is a common cause of ectopic pregnancy. A fertilized egg can get caught in the damaged area of a tube and start to grow there. Some ectopic pregnancies occur without any known cause.
Common causes of fallopian tube damage that may lead to an ectopic pregnancy include:
- Smoking. It raises the risk for ectopic pregnancy. Smoking is thought to damage the fallopian tubes' ability to move the fertilized egg toward the uterus.
- Pelvic inflammatory disease (PID), such as from a chlamydia or gonorrhea infection. PID can create scar tissue in the fallopian tubes.
Some medical treatments can increase your risk. These include:
Prevention
You may be able to prevent an ectopic pregnancy by reducing things that may put you at risk for having one.
Smoking or vaping tobacco increases your risk for ectopic pregnancy. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good.
Try to use safer sex practices, such as using a condom every time you have sex. Use an external condom, which goes on the penis. Or use an internal condom, which goes into the vagina or anus. This will help protect you from sexually transmitted infections (STIs) that can lead to pelvic inflammatory disease (PID). PID is a common cause of scar tissue in the fallopian tubes, which can cause ectopic pregnancy.
If you have one or more risk factors for ectopic pregnancy, you and your doctor can closely monitor your first weeks of a pregnancy.
Learn more
Symptoms
In the first few weeks, an ectopic pregnancy may cause the same symptoms as a normal pregnancy, such as a missed menstrual period, fatigue, nausea, and sore breasts.
The early signs of an ectopic pregnancy are:
- Belly pain or pelvic pain. It most often starts 6 to 8 weeks after a missed period. It may be sharp and on one side at first. And you may have pain during sex.
- Vaginal bleeding. It may be light.
As an ectopic pregnancy progresses or ruptures, other symptoms develop. They include:
- Sudden or severe pain in the belly or pelvis. The pain may progress from one side to your entire belly.
- Shoulder pain caused by bleeding into the belly under the diaphragm. The bleeding irritates the diaphragm and is felt as shoulder pain.
- Heavy or severe vaginal bleeding.
- Dizziness, light-headedness, or fainting (syncope) caused by internal bleeding.
- Signs of shock.
What Happens
Normally, at the start of a pregnancy, the fertilized egg travels from the fallopian tube to the uterus, where it implants and grows. But in a small number of pregnancies, the fertilized egg attaches to an area outside of the uterus. This results in an ectopic pregnancy (also known as a tubal pregnancy or an extrauterine pregnancy).
An ectopic pregnancy cannot support the life of a fetus for very long. But an ectopic pregnancy can grow large enough to rupture the area and cause heavy bleeding, which is dangerous. If you have signs or symptoms of an ectopic pregnancy, you need immediate medical care.
An ectopic pregnancy can develop in different locations. In most cases, the fertilized egg has implanted in a fallopian tube.
In rare cases:
- The egg attaches and grows in an ovary, the cervix, or the abdominal cavity (outside of the reproductive system).
- One or more eggs grow in the uterus at the same time as one or more eggs grow in a fallopian tube, the cervix, or the abdominal cavity. This is called a heterotopic pregnancy.
Getting pregnant after an ectopic pregnancy
It's common to worry about your fertility after an ectopic pregnancy. Having an ectopic pregnancy doesn't mean that you can't have a normal pregnancy in the future. But it does mean that:
- You may have trouble getting pregnant.
- You are more likely to have another ectopic pregnancy.
If you get pregnant again, be sure your doctor knows that you had an ectopic pregnancy before. Regular testing in the first weeks of pregnancy can find a problem early or let you know that the pregnancy is okay.
When to Call a Doctor
If you are pregnant, be alert to the symptoms that may mean you have an ectopic pregnancy, especially if you are at risk. If you have symptoms of or are being treated for an ectopic pregnancy, avoid strenuous activity until your symptoms have been checked by a doctor or midwife.
Call 911 or other emergency services immediately if:
- You passed out (lost consciousness).
- You have severe vaginal bleeding. This means that you are soaking through a pad each hour for 2 or more hours.
- You have sudden, severe pain in your belly or pelvis.
- You feel you cannot stop from hurting yourself or someone else.
Where to get help 24 hours a day, 7 days a week
If you or someone you know talks about suicide, self-harm, a mental health crisis, a substance use crisis, or any other kind of emotional distress, get help right away.
- Call or text Canada's suicide and crisis hotline at 988.
- Call Talk Suicide Canada: 1-833-456-4566 or text 45645 (4 p.m. to midnight ET).
- Go to the Talk Suicide Canada website at https://talksuicide.ca for more information.
Consider saving these numbers in your phone.
Call your doctor, midwife, or nurse advice line now or seek immediate medical care if:
- You are dizzy or light-headed, or you feel like you may faint.
- You have vaginal bleeding.
- You have new cramps or new pain in your belly or pelvis.
- You have new pain in your shoulder.
Examinations and Tests
A urine test can show if you are pregnant. If you have symptoms of a possible ectopic pregnancy, you will have:
- A pelvic exam to check on the size of your uterus and feel for growths or tenderness in your belly.
- A blood test that checks for the level of the pregnancy hormone (hCG). This test is repeated 2 days later. Low or slowly increasing levels suggest a problem, such as an ectopic pregnancy.
- An ultrasound. This test can show pictures of what's inside your belly. With ultrasound, a doctor can usually see a pregnancy in the uterus 6 weeks after your last menstrual period.
During the week after treatment for an ectopic pregnancy, your hCG blood levels are tested several times. In some cases, hCG testing continues for weeks to months until hCG levels drop to a low level.
Learn more
Treatment Overview
In some cases, you may have expectant management. This means your doctor monitors your pregnancy hormone (hCG) levels to check if they are dropping on their own. But in most cases, an ectopic pregnancy is treated right away to avoid rupture and severe blood loss. The decision about which treatment to use depends on how early the pregnancy is found and your overall condition.
Medicine can be used if the pregnancy is found early, before the pregnancy has grown too big. In most cases, one or more shots of a medicine called methotrexate are given. You will need follow-up blood tests for several weeks to make sure the treatment worked.
Surgery may be used if the ectopic pregnancy is found later or is causing internal bleeding or high hCG levels. The surgery may be done through one or more small cuts (incisions) in your belly. If you need emergency surgery, you may have a larger incision.
Learn more
Self-Care
- Rest when you feel tired. You may be more tired than normal for a few weeks.
- Avoid moving quickly or lifting anything heavy until your doctor tells you it is safe to do your normal activities.
- Ask your doctor when you can have vaginal sex again.
- Your doctor might want you to use sanitary pads if you have vaginal bleeding. Using pads makes it easier to keep track of your bleeding.
- If you are treated with methotrexate:
- Follow your doctor's instructions about taking over-the-counter pain medicine, such as acetaminophen. Don't take non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen. Read and follow all instructions on the label.
- Do not take two or more pain medicines at the same time unless the doctor told you to. Many pain medicines have acetaminophen, which is Tylenol. Too much acetaminophen (Tylenol) can be harmful.
- Do not drink alcohol.
- Do not take vitamins that contain folic acid, such as prenatal vitamins.
- Avoid direct sunlight. It can cause skin problems while methotrexate is in your body.
- Avoid foods that may give you gas, such as beans, broccoli, cabbage, and apples.
- Pay attention to your feelings. If you're sad and it's not getting any easier, talk with your doctor or a counsellor.
- Talk to your doctor if you want to try to get pregnant soon. The doctor can tell you when it's safe to do so.
- If you don't want to get pregnant, ask your doctor about birth control. It's possible to get pregnant again before your next period starts.
- Go to all follow-up appointments and tests. This helps your doctor make sure that your pregnancy hormone levels are dropping.
Learn more
Watch
Medicines
A medicine called methotrexate is usually the first treatment choice for an early ectopic pregnancy. Whether medicine can be used depends on how early the pregnancy is found and your overall condition. It is not an option if the pregnancy has grown too big or the fallopian tube has ruptured.
Methotrexate is usually given as one or more shots injected into a muscle. After the shot, you'll need follow-up blood tests for several weeks. These tests are to make sure that the medicine worked.
Methotrexate may cause belly cramps and pain that last a few days. And it can also cause side effects, such as nausea, indigestion, and diarrhea.
For an ectopic pregnancy that is more developed, surgery is a safer and more dependable treatment. Sometimes methotrexate is used after surgery. It's to make sure that all ectopic cell growth has stopped.
Surgery
Surgery is the fastest way to treat an ectopic pregnancy. The two types of surgery are:
- Salpingostomy.
The doctor removes the ectopic growth through a small cut in the fallopian tube. This is called linear salpingostomy. The cut is left to close by itself. Or it may be stitched closed.
- Salpingectomy.
The doctor removes a part of the fallopian tube. The remaining healthy fallopian tube may be reconnected. This surgery is needed when the fallopian tube is so stretched that it may rupture. It's also used when the tube has already ruptured or is very damaged.
These surgeries can be done in two ways. The first is through a small incision using laparoscopy. The second is called laparotomy. It's done through a larger incision in the belly. Laparoscopy takes less time than laparotomy. And the hospital stay is usually shorter.
If the fallopian tube that isn't part of the ectopic pregnancy is healthy, then both surgeries have about the same effect on future fertility. But if that other fallopian tube isn't healthy, then your doctor may try to do a salpingostomy.
Learn more
Credits
Adaptation Date: 06/15/2023
Adapted By: Alberta Health Services
Adaptation Reviewed By: Alberta Health Services
