Learning About ICD Shocks
What are ICDs and ICD shocks?
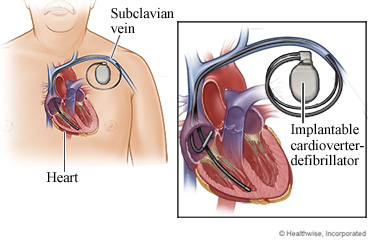
An implantable cardioverter-defibrillator (ICD) is a device that is placed under the skin of your chest. It has one or two thin wires (called leads). With some ICDs, these leads are placed inside the heart. Other ICDs have a lead that is placed under the skin so that it lies near your heart. The ICD is always checking your heart for a life-threatening rapid heart rhythm. The ICD may try to slow the rhythm back to normal using electrical pulses. If the dangerous rhythm does not stop, the ICD sends an electric shock to the heart to restore a normal rhythm. The device then goes back to its watchful mode.
The idea of living with an ICD and getting shocked worries some people. The shock can be uncomfortable. It may feel like you are being kicked in the chest. For many people, getting a shock can cause anxiety and depression.
It's normal to be worried about living with an ICD. After all, you don't know when a shock might occur, and a shock could be a reminder that your heart is not as healthy as it could be.
But an ICD is an important part of your treatment. It can save your life. If you take a few simple steps, you can feel better about having an ICD.
How can you prepare for an ICD and ICD shocks?
Know your ICD treatment
- Learn how the ICD works, what it does, and how it keeps you safe. This can help reduce any anxiety you may feel.
- Keep your regular doctor appointments. Your doctor:
- Sets both the rate at which a shock will occur and the level of shock needed to restore your heart to a normal rate.
- Checks to see whether the ICD has given you any shocks since your last visit. This helps your doctor know if your medicines need to be adjusted.
- Checks the ICD battery.
- Talk with others who have an ICD. Ask them if they have been shocked and what it was like. Ask them how they cope with it. Talking with others can help you feel better.
- Always carry your ICD identity card, a list of all the medicines you are taking, and your doctor's name and phone number. This will help you get the best possible treatment if you get a shock and need help.
Make an action plan
Talk to your doctor about making an action plan for what to do if you get shocked. Here is an example:
- After one shock:
- Call 911 or other emergency services right away if you feel bad or have symptoms like chest pain.
- Call your doctor soon if you feel fine right away after the shock. Your doctor may want to talk about the shock and schedule a follow-up visit.
- If you get a second shock in a 24-hour period, call your doctor right away. Call even if you feel fine right away.
Stay calm after a shock
- Follow the action plan you made with your doctor.
- Do some breathing exercises. They may help you relax.
- Sit or lie in a comfortable position. Put one hand on your belly just below your ribs and the other hand on your chest.
- Take a deep breath in through your nose, and let your belly push your hand out. Your chest should not move.
- Breathe out through pursed lips as if you were whistling. Feel the hand on your belly go in, and use it to push all the air out.
- Breathe in and out like this until you feel more relaxed.
- Don't make changes in what you do. You may want to avoid an action because you think it caused the shock. But a shock can occur at any time, and you can't prevent shocks by your actions alone. Don't stop doing things you enjoy to try to avoid a shock.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor or nurse advice line (811 in most provinces and territories) if you are having problems. It's also a good idea to know your test results and keep a list of the medicines you take.
Where can you learn more?
Go to https://www.healthwise.net/patientEd
Enter F645 in the search box to learn more about "Learning About ICD Shocks".
Current as of: July 31, 2024
