Indwelling Catheter Drainage for Chest or Abdomen: Care Instructions
Overview
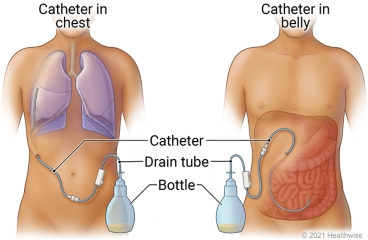
An indwelling chest or belly (abdominal) catheter is a soft, flexible tube that runs under your skin to an area next to your lungs or in your belly. One end of the tube stays outside your body and drains into a bottle or other container.
When fluid builds up around your lung (pleural effusion), it can cause discomfort and make it hard for you to breathe. Other symptoms can include fever or cough.
When fluid collects in the space between the organs in your belly and the belly wall (ascites), you may feel bloated or overly full. Other symptoms of ascites (say "uh-SY-teez") include belly pain and weight gain.
Draining the fluid through a tube helps relieve these symptoms.
"Indwelling" means the tube stays in place for as long as you need it. You don't have to get a new catheter put in every time fluid builds up. You can empty the fluid from the bottle at home—or have someone else do it—whenever you need to.
The doctor may use stitches to hold the catheter in place where it exits your body. The site may be sore for a day or two.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor or nurse advice line (811 in most provinces and territories) if you are having problems. It's also a good idea to know your test results and keep a list of the medicines you take.
How can you care for yourself at home?
- Follow the instructions for taking care of your catheter. Your doctor or nurse will teach you or your caregivers what to do.
How to drain fluid
- Wash your hands well. Clean your work area with a disinfecting wipe or alcohol. Place everything you will need on your work area, including the drain tube and the bag or bottle that will collect the fluid.
- Wear disposable gloves if they are part of your kit or if your doctor told you to.
- Make sure the drainage tube is closed. It may have a clip on it.
- Remove the cap at the end of your catheter. Wipe the end of the catheter and the end of the drain tube with alcohol.
- Attach the catheter to the drain tube.
- Make sure the bottle or bag is at least an arm's length below your chest or belly. If your system is vacuum-sealed or uses a pump, you may not need to lower the container.
- Depending on what type of drainage kit you have, push the plunger or squeeze the pump to start the drainage. Some kits include a clamp you need to release before the drainage starts.
- Your doctor will tell you how much fluid to drain at one time. In general, don't drain more than 1,000 millilitres (mL) from your chest or more than 2,000 mL from your belly in a 24-hour period.
- If you feel pain during drainage, you may be able to ease the pain by slowing down the drainage rate. Do this by raising the bag or bottle. Some drainage kits include a clamp you can pinch to slow the drainage.
How to empty the drainage bag or bottle
- Disconnect the drain tube from your catheter. Let all the fluid in the drain tube flow into the bag or bottle.
- Wipe the end of your catheter with alcohol. Put a new valve cap on the catheter, and make sure it's tight.
- Tape the end of the catheter to your skin wherever it's most comfortable.
- Empty the bag or bottle into the toilet or sink.
- If you spill some fluid on clothes or skin, clean it up with soap and warm water. You may want to use bleach for spills on some surfaces.
- Keep a drainage record sheet so that your doctor can see how much fluid is coming from the tube. Your doctor or nurse will give you a record sheet. Or you can just write down the date, time, amount, and colour of the drainage. Save the record sheet to show to your doctor.
How to change the bandage (dressing)
- Follow your doctor's instructions for how often to change the bandage.
- Carefully remove the bandage.
- Check your skin for signs of infection.
- Clean the skin with an alcohol pad.
- Open a new dressing kit.
- Put the first layer of gauze or foam on the skin, under the catheter. Put the second layer on top of that. Put the clear sticky bandage over everything.
When should you call for help?
Call 911 anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have severe trouble breathing.
Call your doctor or nurse advice line now or seek immediate medical care if:
- You have new or worse trouble breathing.
- You have symptoms of infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the area.
- Pus draining from the area.
- A fever.
- You have new or worse pain.
- The fluid looks different from what you normally see.
- The tube comes out of your body.
Watch closely for changes in your health, and be sure to contact your doctor or nurse advice line if:
- There is little or no fluid draining from the catheter.
- You do not get better as expected.
Current as of: October 24, 2024
