Vaginal Bleeding During Pregnancy: Care Instructions
Overview
It's common to have some vaginal bleeding in the first trimester (3 months) when you are pregnant. In some cases, the bleeding isn't serious if there aren't any more problems with the pregnancy.
But sometimes heavy or painful bleeding in the first trimester is a sign of more serious problems including miscarriage and ectopic pregnancy.
Bleeding in the second or third trimester may be a sign of more serious problems. This could include a problem with the placenta and a higher chance of preterm labour and birth.
If vaginal bleeding happens after 20 completed weeks of pregnancy, it’s called antepartum hemorrhage (antepartum – during pregnancy, hemorrhage – bleeding doesn’t stop or is too much).
The most common causes of antepartum hemorrhage are:
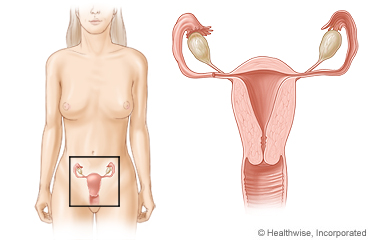
- Placental abruption – part of the placenta separates from the wall of the uterus.
- Placenta previa – the placenta has attached so low that it blocks or partially blocks the opening of the uterus (cervix).
- Bleeding from the cervix or vagina.
You may have to see your healthcare provider or midwife more often to be sure everything is okay. You may also need more tests to find the cause of the bleeding.
Home treatment may be all you need. But it depends on what is causing the bleeding. Be sure to tell your healthcare provider or midwife about all your concerns.
If you have any new symptoms or your symptoms get worse, get medical treatment right away.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your healthcare provider or nurse advice line (811 in most provinces and territories) if you are having problems. It's also a good idea to know your test results and keep a list of the medicines you take.
How can you care for yourself at home?
- Watch for bleeding and signs of preterm labour.
- If your healthcare provider or midwife prescribed medicines, take them exactly as directed. Call your healthcare provider, midwife, or nurse advice line if you think you are having a problem with your medicine.
- Do not have sexual intercourse unless your healthcare provider or midwife says it's okay.
- Do not put anything in your vagina until your healthcare provider or midwife says it's okay.
- In your third trimester, follow your healthcare provider’s instructions about how often to count your baby’s movements. For information on counting your baby’s movements, go to: Fetal Movement Count Chart (albertahealthservices.ca).
- Talk to your healthcare provider about when you can go back to your routine activity or light exercise.
- Take time every day to relax, rest, and get enough sleep. Nap if you need to.
- Eat a healthy and well-balanced diet that includes peas, beans, and leafy green vegetables. Talk to a dietitian if you need help planning your diet.
- Do not use tobacco or tobacco-like products, including cannabis, and other substances. They can harm your health. They can also affect your baby’s growth, health, and the development of their brain and lungs. If you need help to use less or quit, talk to your healthcare provider, or go to the Alberta Quits website.
- Do not drink alcohol. Alcohol affects everyone differently and may be a risk to your health. Alcohol passes through the placenta to your baby and can cause problems with your baby’s growth, health, and development.
Pregnancy can be an emotional and unpredictable time. When you have complications in your pregnancy you may have more stress. This can lead to other concerns for you and your family. Talk to your healthcare provider about how you’re feeling and any other concerns you have.
When should you call for help?

Share this information with your partner or a friend. They can help you watch for warning signs.
Call 911 anytime you think you may need emergency care. For example, call if:
- You have sharp or sudden, severe pain in your belly or pelvis that doesn’t get better or go away.
- You passed out (lost consciousness).
- You have severe or a steady flow of vaginal bleeding. This means you are soaking through a pad each hour for 2 or more hours.
Call your healthcare provider, midwife, or nurse advice line now or seek immediate medical care if:
- You have any vaginal bleeding during pregnancy.
- You are dizzy or light-headed, or you feel like you may faint.
- You have a fever.
- You have new or worse pain in your belly, pelvis, vaginal area or lower back.
- You have a sudden release of fluid from your vagina.
- You think that you are in labour or are having contractions of your uterus with or without pain (6 or more in 1 hour).
- You are in your third trimester, and you notice that your baby has stopped moving or moves less than 6 times in 2 hours.
Watch closely for changes in your health, and be sure to contact your healthcare provider, midwife, or nurse advice line if you have any problems.
Adaptation Date: 10/11/2023
Adapted By: Alberta Health Services
Adaptation Reviewed By: Alberta Health Services
