MRI and Ultrasound Guided Biopsy of the Prostate
Care instructions
Why is this test done?
A biopsy is a procedure that takes a sample of tissue for study. The most common reason is to look for cancer.
The prostate is part of the male reproductive system. It produces a fluid that makes up most of what’s in semen.
For MRI and ultrasound prostate biopsies, you will have imaging done to identify specific areas for the biopsy. The imaging might include:
an MRI first (1 week before your biopsy), then an ultrasound during the biopsy
an MRI and ultrasound at the same time (fusion)
Using advanced biopsy equipment, the MRI images combine with ultrasound images to identify specific areas for biopsy of the prostate.
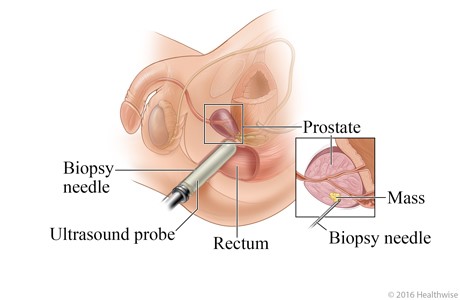
A prostate biopsy is done with a biopsy needle. The needle removes a small sample of tissue from the prostate for testing. With an MRI and ultrasound guided biopsy, the needle can be placed more accurately with the help of the combined images.
A prostate biopsy is usually done if:
you have a high or rising prostate-specific antigen (PSA) level
your healthcare provider thinks that you may have prostate cancer
you’ve had an abnormal rectal exam
you’ve had abnormal findings on a prostate MRI
your genes put you at more risk to develop prostate problems
you’re being monitored for prostate cancer
What are the benefits?
Some abnormal tissue growths (called tumours) that can grow in your prostate are clinically insignificant. This means that they don’t need any immediate treatment. They aren’t likely to pose a threat to your health.
Using the MRI image to guide your biopsy helps raise the chance of finding prostate tumours that do need treatment.
MRI images give precise information. This lowers the chance that a serious tumour will be missed, which can happen with a regular ultrasound biopsy.
What are the risks?
After this procedure you may have:
difficulty peeing (in rare cases, you may need a temporary urinary catheter)
bleeding in your stool (poop), urine, and semen
infection in the blood or urine
pain (usually very little)
allergic reaction
Getting ready for your procedure
MRI
Before your MRI:
Get your bloodwork for creatinine level done at least 6 weeks before your MRI appointment.
The diagnostic imaging department will call you to confirm your instructions 48 hours before your appointment. Make sure you understand these instructions and follow them carefully. Ask the diagnostic imaging department any questions you might have.
You may be asked to use an enema the night before and the morning of the MRI. It’s important that your bowels are empty.
Only have clear liquids after dinner the night before your MRI.
Prostate biopsy procedure
Your urine may be tested to see if you have a urinary tract infection. If you have a urinary tract infection, your prostate biopsy may be postponed while you take antibiotics to clear the infection.
Follow the instructions you get to stop taking medicines before the procedure that can put you at higher risk of bleeding. This includes medicines such as warfarin (Coumadin), clopidegrel (Plavix), rivaroxaban (Xarelto), Aspirin, ibuprofen (Advil, Motrin), and certain herbal supplements. Talk with your urologist about any blood thinners you take. You can take all other medicines as you normally would.
You will have a cleansing enema before your biopsy procedure.
For information about what you can eat before the biopsy procedure, check with the facility where your procedure has been scheduled.
Take your antibiotics as you were instructed. This helps to prevent infection from the procedure.
What happens during the procedure?
MRI and ultrasound guided prostate biopsy is usually done in the outpatient procedure area. This means that you will not stay overnight in the hospital. The MRI and ultrasound images help guide where the biopsy needle is put in.
You’ll be asked to lay on your left side. The doctor will examine your prostate again. A lubricated ultrasound probe is then placed into your rectum. The ultrasound scan of your prostate is done.
You may feel some discomfort or mild pain when the ultrasound probe is put into your rectum. Your healthcare team will use local anesthesia (numbing medicine) to ease the discomfort. You may also be given medicine to make you sleepy and comfortable during the test.
The biopsy (tissue sample) is taken using a needle and then sent to the lab for analysis.
What will happen after?
Arrange to have someone take you home. Some medicines you get during the procedure will make it unsafe for you to drive or to get home on your own.
It’s common to have pain in your rectum or discomfort for a few days.
Your biopsy results should be available about 2 weeks after your procedure. You’ll have a follow-up appointment with your urologist.
Caring for yourself after your biopsy
Take your antibiotics as prescribed.
Don’t take any anti-inflammatory medicines such as ibuprofen (Advil, Motrin) for about 1 week after your biopsy. Your urologist will let you know when you can start taking this type of medicine again.
You may see blood in your urine, stool, or semen for up to 6 to 8 weeks after your biopsy.
If you have pain, sit in a tub of warm water and take acetaminophen (Tylenol) as prescribed.
You can eat your normal diet. If your stomach is upset, try bland, low-fat foods like plain rice, broiled chicken, toast, and yogurt.
Drink plenty of fluids unless your doctor tells you not to.
Avoid drinks with caffeine or alcohol, and don’t have spicy foods that may irritate the biopsy area.
Rest when you feel tired. Getting enough sleep will help you recover.
Try to walk each day. Start by walking a little more than you did the day before. Bit by bit, increase the amount you walk.
Go back to your regular physical activities as your pain level allows. Follow the instructions about the activity and, if you need it, take pain medicine as prescribed.
Avoid strenuous exercise and sex for 2 days after your biopsy.
Call your doctor or go to the emergency department if you have signs of infection such as:
If you have any concerns or questions about your procedure, call your doctor.
To see this information online and learn more, visit MyHealth.Alberta.ca/health/pages/conditions.aspx?Hwid=custom.ab_mriusfusionguidedbiopsy_prostate_inst.
For 24/7 nurse advice and general health information call Health Link at 811.
Current as of: November 19, 2024
Author: Diagnostic Imaging, Alberta Health Services
This material is not a substitute for the advice of a qualified health professional. This material is intended for general information only and is provided on an "as is", "where is" basis. Although reasonable efforts were made to confirm the accuracy of the information, Alberta Health Services does not make any representation or warranty, express, implied or statutory, as to the accuracy, reliability, completeness, applicability or fitness for a particular purpose of such information. Alberta Health Services expressly disclaims all liability for the use of these materials, and for any claims, actions, demands or suits arising from such use.
