The Heart Surgery Recovery Pathway
The
Heart Surgery Recovery Pathway shows what to expect while you’re in hospital and once you’re home.
Ask for pain medicine before the pain gets too bad.
When your pain is being managed, it’s easier to do your deep breathing and coughing exercises to keep your lungs clear.
You’ll also be able to move around better to prevent blood clots.
Managing pain
It’s important that you’re as comfortable as possible.
Most people find their pain can be managed by oral pain medicine once they can have fluids.
You may be asked to rate your pain on a pain scale where 0 means no pain and 10 is the worst pain you can imagine.
Tell your nurse if your pain reaches a 4 or isn’t being helped by the pain medicine.
Breathing exercises (deep breathing and coughing)
Deep breathing, coughing, and getting up to move soon after surgery lowers the risk of pneumonia and blood clots. It’s uncomfortable to do at first, but it does get easier.
The physical therapist and nurse will ask you to do deep breathing and coughing exercises. Try to take 10 slow, deep breaths every hour followed by good strong coughing.
To protect your chest incision, you’ll be given a pillow or flannel blanket to hold. You can hold your support pillow or blanket against your chest incision when you cough or sneeze.
If you cough up some mucus, clear it into a tissue, and repeat the cough until no more mucus is coming up.
Your incisions
The dressing on your chest and on your arm or leg (if you had a CABG) may be taken off after 2 or 3 days. Some dressings will stay on longer.
Your healthcare team will clean your incision and put on a new dressing as needed.
To help stop germs from spreading to your incision, clean your hand with the alcohol-based hand rubs (hand sanitizer) you can find all over the hospital. Or you can wash your hands well with soap and water.
If you aren’t sure if your healthcare provider has cleaned their hands, it’s okay to ask them to clean their hands.
It's normal for incisions to:
- look slightly red
- feel tender, uneven, bumpy, numb, tight, like they're pulling, or itchy
- drain a small amount of clear or yellow fluid
Showering
You can take a shower when you're ready. Make sure the water isn't too hot.
Don’t aim the spray at your incisions. Let the water flow over your incisions without soaking them.
Gently pat the incisions dry. Don’t rub them.
Caring for your bowels
Even though you haven’t eaten much, you may feel full a few days after your surgery. You’ll be given stool softeners or a laxative to help your bowels to move. Tell your nurse if the softener or laxative doesn’t help.
You need to have at least 1 bowel movement before you’re discharged from hospital.
Nutrition
Your body needs more protein and other nutrients to help you heal after surgery.
It’s common not to feel hungry for as long as 10 days after surgery. Even though you may not feel like eating, it’s important that you do.
Ask to speak to a dietitian if you have questions about food or are worried about not feeling hungry.
Your diet will be changed from fluids to more solid food depending on how you feel. Your doctor may put you on a low salt diet while you’re in the hospital.
Activity after surgery
You need to move your body after surgery.
During your hospital stay, you will aim to walk 4 to 6 times a day in the hallway. You will also start doing your recovery exercises. Walking and the exercises will help with stiffness and feeling sore and get your full muscle movement back.
Once you're home, you'll have the goal of walking a little more each day as you recover.
Keep Your Move in the Tube
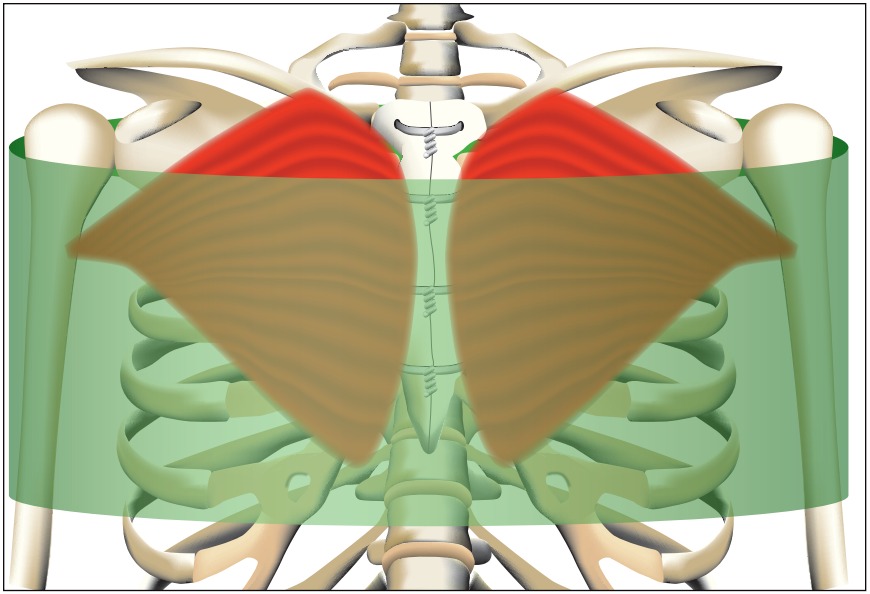
Keep Your Move in the Tube is a movement guideline that helps you protect your breastbone (sternum) while it heals.
Imagine your upper body is inside a big tube, as in the image below. This will help you focus on keeping your upper arms close to your body when your movement includes pushing, pulling or lifting.
Credit: ©2018 Baylor Health Care System
You'll know when it's safe to move more by paying attention to how much pain or discomfort you feel.
You can slowly start to move out of "the tube" with your arms when you no longer have much pain or discomfort.
For some people supporting the breasts by wearing a chest binder or front-closing bra may help lower pain or discomfort after surgery and chest discomfort while you're healing. Your surgeon will recommend what is best for you.
