What
is an intrauterine
device (IUD)?
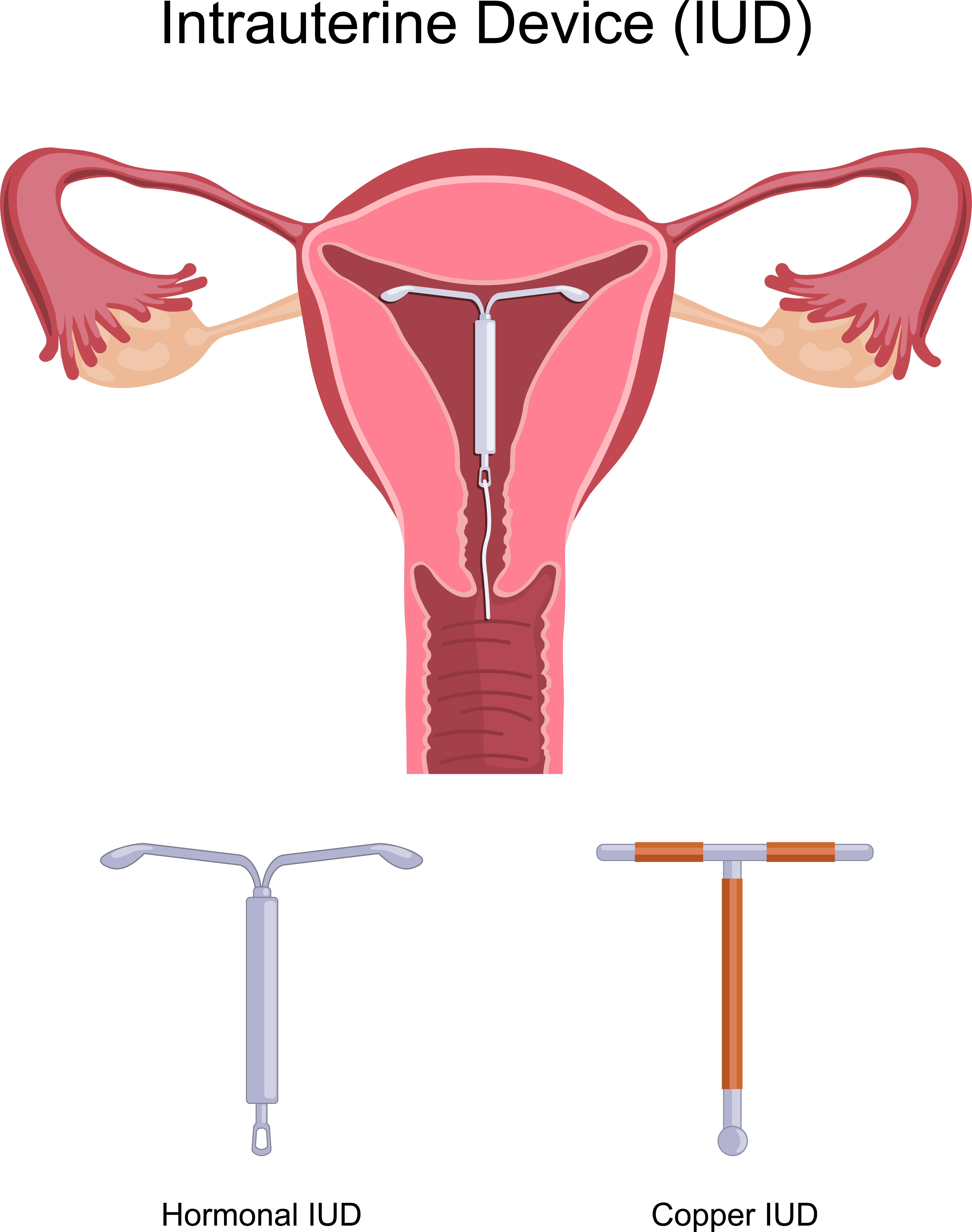
An IUD is a small, soft, T-shaped device with a nylon string attached to it. It is put in the uterus by a health care provider to help prevent pregnancy.
The IUD prevents pregnancy by stopping the egg and sperm from meeting. If the sperm and egg don't meet, pregnancy can't happen.
There are 2 types of IUDs:
- copper (like Mona Lisa®, Liberté®, Flexi-T®, SMB®). Various options have different shapes, sizes, copper dosages, and materials (like silver and nickel).
- hormonal (like Mirena® or Kyleena®). These are also known as a hormonal intrauterine system.
Copper IUD
- has a copper wire wrapped around it
- slows the sperm movement, so it is harder to get to the egg
- decreases the ability of the sperm to fertilize the egg
- changes the lining of the uterus to stop a fertilized egg from growing inside the uterus
Depending on the type of copper IUD, it can help prevent pregnancy for 3 to 10 years. It can also be used as emergency contraception up to 7 days after vaginal sex without a condom.
Hormonal IUD
This IUD has a hormone (levonorgestrel) wrapped around it that is slowly released into the uterus. The IUD:
- thickens the mucous in the cervix, so it is harder for the sperm to get to the egg
- slows the sperm movement, so it is harder to get to the egg
- changes the lining of the uterus to stop a fertilized egg from growing inside the uterus
- may stop the ovaries from releasing an egg
The hormonal IUD can help prevent pregnancy for up to 5 years. You can talk to your health care provider about possible longer use depending on your age and the product you have.
How well do IUDs work?
How do I start using IUD?
Before you get an IUD, get checked for STIs. The IUD is put in (inserted) by your health care provider. A health care provider can discuss how to check the IUD strings.
When does the IUD start working?
The copper IUD protects you from pregnancy as soon as it is inserted.
If a hormonal IUD is put in on:
- day 1 to 5 of your period, or if you are inserting a new IUD before your old one expires, it works right away to prevent pregnancy
- any other day, use an extra method of birth control (like condoms) or don’t have vaginal sex for
7 days
What are the benefits of an IUD?
- An IUD can help prevent pregnancy for up to 10 years (depending on type).
- If you want to get pregnant, your health care provider can take out your IUD at any time.
- IUDs can lower the risk of having cancer of the uterus.
- If you can’t use birth control with estrogen, you can use an IUD.
- If you cannot be on any form of hormonal medication, you can use a copper IUD.
- The hormonal IUD may make your periods lighter, or you might even stop having periods. It might also make your period cramps less painful.
How will an IUD affect my period?
Most people will experience changes to their period. These changes are not harmful and do not affect how well the IUD works. The kind of changes depend on the type of IUD.
The copper IUD may cause:
- more bleeding and cramping with your period (which may get better over time)
- longer periods
Mirena® hormonal IUD:
- may cause spotting for 3 to 6 months after it is inserted
- after 3 to 6 months, usually makes periods much lighter
- after 12 months, 16% of people with a Mirena® stop getting a period, and 57% have infrequent bleeding
Kyleena® hormonal IUD:
- may cause spotting for 3 to 6 months after it is inserted
- after 12 months, 12% of people with a Kyleena® stop getting a period
What are the side effects of an IUD?
With the hormonal IUD, there is a chance (especially in the first few months) that you may have:
- headaches
- tender breasts
- acne
- mood changes
What are the disadvantages of having an IUD?
There is a 2% to 10% chance of the IUD falling out. This happens most often in the first year. This risk is greater if the IUD was inserted right after you had a baby, or if you’ve had an IUD fall out before.
It is rare to get pregnant with an IUD. If you do get pregnant with an IUD, there is a higher risk of:
- a pregnancy outside the uterus (ectopic pregnancy)
- miscarriage
The risk of
pelvic inflammatory disease (PID) may be higher during the first month with an IUD.
In rare cases, an IUD can make a hole in the wall of the uterus when it is being inserted. If this happens, you may need a minor surgery to take it out.
Insertions may cause discomfort or pain. Talk to your health care provider about ways to make insertion more comfortable.
I'm thinking of getting an
IUD.
What do I need to
tell my healthcare provider?
If you are thinking of getting an IUD, tell your healthcare provider if you:
- are pregnant or think you might be
- have an STI
- have ever had PID
- have an allergy to copper
-
have or have had breast, cervix, or uterine cancer
-
have irregular vaginal bleeding or don’t have your period
I have an
IUD. When do I need to contact my healthcare provider?
Contact your healthcare provider if you have an IUD and you:
- think you are pregnant
- have heavy vaginal bleeding
- have lots of abdominal cramping
- can’t find your strings, the strings are longer or shorter, or you can feel your IUD
- think you have been exposed to an STI
- have pelvic pain or vaginal discharge with or without a fever or chills
- have pain with sex
- have any questions or other problems with your IUD
- want to remove your IUD
If you think your IUD isn't working and you've had vaginal sex without a condom, think about getting
emergency contraception as soon as possible.
What else is important to know about consent, sexual activity, and birth control?
- You have the right to decide to have sex or not. Talk with your partner or partners about consent.
- There’s an 85% chance of becoming pregnant within one year, if no birth control is used for vaginal sex.
- Use a condom or barrier every time you have sex (oral, vaginal, anal). Condoms help prevent pregnancy, STIs, and HIV.
- You can lower your risk of HIV by taking an HIV prevention pill every day. Many Albertans can get it for free. Visit
HIV PrEP to find out more.
- Transgender and gender diverse people who have a uterus can use hormonal birth control. It can help prevent pregnancy and make periods lighter and less painful.
Where can I find more information?
If you have questions, need to find a sexual health clinic near you, or want more information, call Health Link at 811 anytime, day or night, to talk to a registered nurse.
